The Silent Threat: Understanding Septal Infarct and its Implications
Septal infarct endangers the heart. A coronary artery blockage disrupts blood flow to the septum, the muscular wall that separates the left and right sides of the heart. Oxygen and nutrients are blocked from reaching the septum, causing tissue damage and problems.
Septal infarct must be detected and treated early. Understanding the causes, risk factors, and symptoms of this disorder can help people recognize the signs and seek medical attention.
This article examines septal infarction’s effects on cardiac function and prognosis. We study heart anatomy, infarction mechanisms, and septal infarct detection methods. We also address drugs, surgery, rehabilitation, and lifestyle changes for managing this illness.
We also discuss septal infarct consequences, prevention, and its link to other cardiac disorders. We also discuss the emotional and psychological effects of septal infarct on quality of life, using case studies and personal experiences.
Readers will understand septal infarct after reading this article, enabling them to protect their heart health and make informed medical decisions.
Understanding the Heart’s Anatomy
To understand septal infarct, you need to know cardiac anatomy. The heart circulates oxygen-rich blood throughout the body. It has two ventricles and two atria.
The heart’s septum is vital. The heart’s muscular wall separates oxygenated and deoxygenated blood. Interatrial and interventricular septums separate the atria and ventricles, respectively.
Septal infarction emphasizes the interventricular septum. It distributes blood oxygenated by the left ventricle. When coronary arteries are blocked in a septal infarct, the interventricular septum loses blood supply, causing tissue damage and impairing its function.
Understanding the heart’s complex structure helps people grasp the septal infarct’s effects and the need of maintaining the septum’s health.
The Mechanism of Infarction
Understanding how septal infarction affects the heart requires understanding its mechanism. A blocked coronary artery supplies oxygenated blood to the heart muscle, causing septal infarction.
Plaques, fatty deposits on artery walls, cause coronary artery obstruction. Plaques can break, causing blood clots that block heart blood flow. Blockages in the septum’s coronary arteries impede oxygen and nutrition delivery.
Ischemia occurs when blood flow to the septum is cut off. If blood flow is not restored, septal tissue will perish from a lack of oxygen and nutrients.
Septal infarction can be serious. Chest pain, shortness of breath, and exhaustion might result from a damaged septum. Septal infarction can harm the heart if not diagnosed and treated quickly.
Risk Factors for Septal Infarct
Risk factors increase the likelihood of septal infarction, a dangerous heart disorder. Understanding these risk variables can help identify septal infarct victims and lessen their risk.
Age/Gender Considerations:
Age increases septal infarct risk. Age narrows and stiffens arteries, making blockages more likely.
Septal infarct risk is higher in men. Hormonal changes increase risk after menopause.
Cardiovascular Diseases:
Cardiovascular disease increases septal infarct risk. Hypertension, diabetes, and coronary artery disease can obstruct arteries with plaque.
Diet and lifestyle:
Septal infarction is increased by unhealthy lifestyle choices. Smoking, inactivity, and excessive alcohol usage increase the risk of atherosclerosis.
A diet high in saturated fats, cholesterol, and sodium can cause coronary artery plaques and septal infarction. Recognizing these risk factors helps people make educated lifestyle choices and seek appropriate medical care. A heart-healthy lifestyle, regular checkups, and controlling preexisting diseases can lower septal infarct risk and improve cardiovascular health.
Symptoms and Clinical Presentation
Recognizing the symptoms and clinical presentation of septal infarction is crucial for early detection and timely intervention. Being aware of these signs allows individuals to seek prompt medical attention, which is vital for managing septal infarct effectively.
Chest Pain and Discomfort:
Chest pain is one of the primary symptoms of septal infarction. People may feel chest pressure, tightness, or heaviness.
Discomfort or pain may radiate to the left arm, shoulder, jaw, or back. Not all septal infarcts cause severe chest pain and symptoms can vary.
Shortness of Breath and Fatigue:
Septal infarct can lead to shortness of breath, even with minimal exertion. People may have trouble breathing.
Fatigue and a general feeling of weakness can accompany septal infarct. Individuals may find themselves easily exhausted, even with routine activities.
Additional Signs to Watch For:
Other signs that may indicate septal infarct include dizziness, lightheadedness, and fainting episodes.
Nausea, indigestion, and cold sweats can also be associated with symptoms.
In some cases, individuals may exhibit abnormal heart rhythms or palpitations.
Note that these symptoms might vary from person to person, and some people may have no symptoms at all.
If there is a suspicion of septal infarction or any concerning symptoms, it is crucial to seek immediate medical attention to evaluate the condition and initiate appropriate treatment.
Diagnostic Techniques
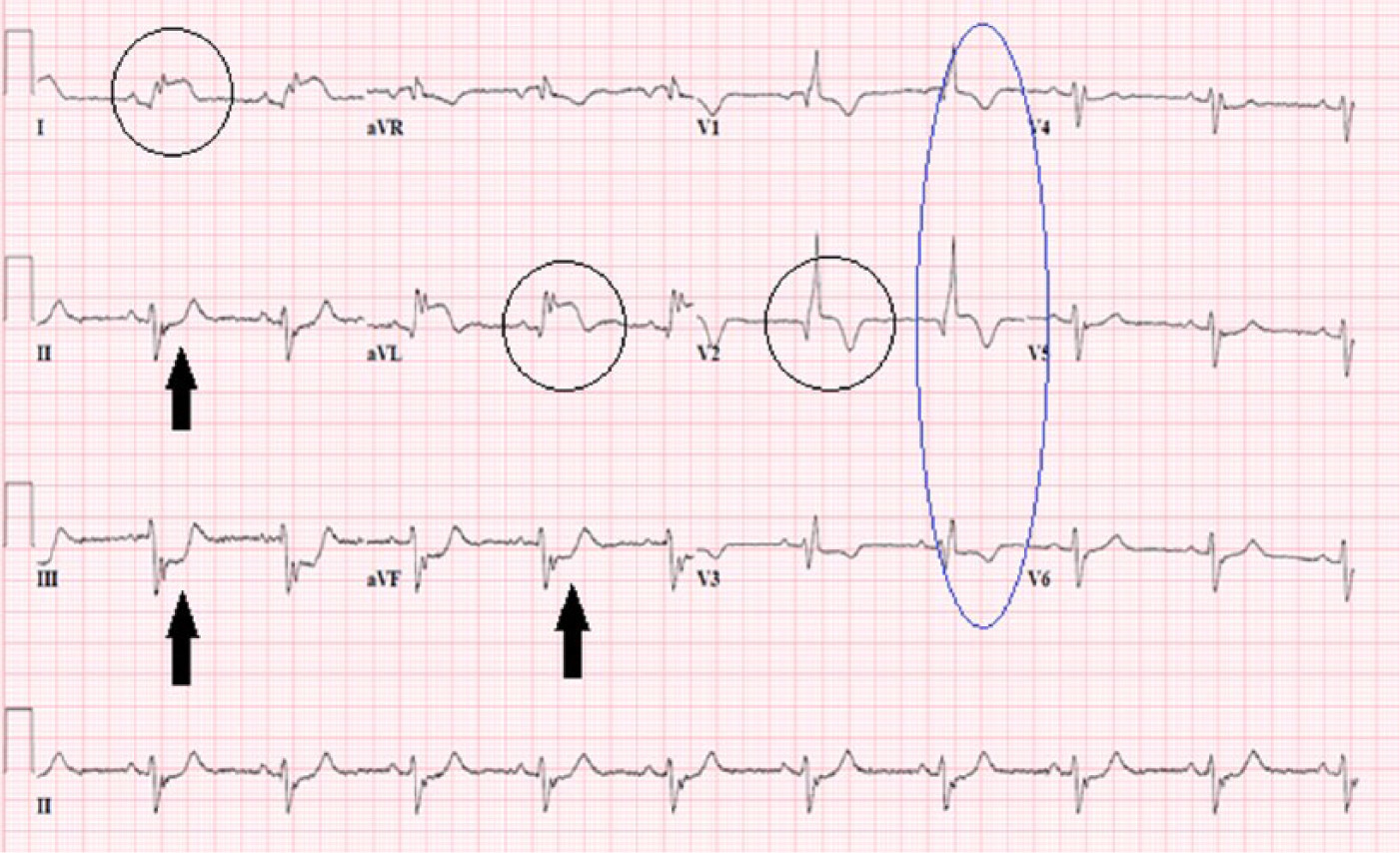
Diagnostic methods help diagnose and treat septal infarction. These methods reveal septum and heart health. ECGs are important diagnostic tools. Healthcare providers can diagnose cardiac rhythm and conduction issues with an ECG. ECG changes like ST-segment elevation or depression may suggest septal infarct. Echocardiography also employs ultrasonic waves to visualize the heart’s architecture, particularly the septum. It helps detect septal anomalies and tissue damage by revealing its size and function. Heart and septum pictures can also be obtained via cardiac magnetic resonance imaging (MRI) or computed tomography (CT) scans. These diagnostic methods including a detailed medical history and symptom evaluation can diagnose septal infarct and guide treatment.
Treatment Options
Septal infarct treatment reduces septum damage, manages symptoms, and improves heart function. Treatment depends on severity and patient characteristics. Septal infarct management requires medications. Aspirin or anticoagulants can prevent blood clots and blockages.
To improve cardiovascular health, blood pressure, cholesterol, and other disorders like diabetes may be treated with medications. Medical procedures may be needed. Revascularization treatments like PCI or CABG can unblock coronary arteries to restore blood flow to the septum. If difficulties or septum damage occur, surgery may be considered. Treatment also includes lifestyle changes like eating a heart-healthy diet, exercising regularly, stopping smoking, and managing stress.
Cardiac rehabilitation programs can assist with lifestyle adjustments. Septal infarct treatment requires a personalized combination of drugs, treatments, and lifestyle changes to promote heart health and well-being.
Prevention Strategies
Preventing septal infarct includes taking preventative steps. Prevention can protect heart health and reduce septal infarct risk.
Managing Risk Factors:
Prevention requires risk factor management. This includes a balanced diet reduced in saturated fats, cholesterol, and sodium.
Regular exercise and stopping smoking reduce septal infarct risk. Exercise improves cardiovascular health and blood pressure.
Meditation and yoga can reduce stress and heart disease risk.
Heart Checkups:
Preventing septal infarction requires regular cardiology checkups. Checkups assess blood pressure, cholesterol, and heart health.
Routine screenings can detect early warning symptoms and help people manage underlying diseases like hypertension and diabetes that may cause septal infarction.
Health Education:
Preventing septal infarction requires heart health education. Knowledge helps people decide and act.
Understanding cardiovascular symptoms, risk factors, and lifestyle changes might drive people to prioritize their heart health.
Health education, community programs, and informational resources can spread accurate information and encourage prevention.
Controlling modifiable risk factors, prioritizing cardiovascular checkups, and boosting health education and awareness can lower septal infarct risk. Prevention helps the heart and general wellness.
Septal Infarct and Other Heart Conditions
Septal infarct, a kind of myocardial infarction, can be linked to other heart disorders, revealing the interconnectedness of cardiac health and function. Septal infarct diagnosis, treatment, and management require understanding these linkages.
Related Myocardial Infarctions:
Myocardial infarction—the destruction of cardiac muscle tissue owing to inadequate blood supply—includes septal infarction. The septum—the muscle wall that divides the heart—is damaged.
Septal infarct can occur alongside other myocardial infarctions, such as anterior or inferior infarctions, which affect other heart muscle sections. Infarction severity and location can affect cardiac function.
Cardiovascular disease:
Coronary artery disease (CAD), which narrows or blocks heart-supplying coronary arteries, is typically linked to septal infarct. CAD reduces septal blood flow, increasing septal infarct risk.
Atherosclerosis—plaque buildup in the arteries—may increase the risk of septal infarction in CAD patients. Blood clots can block septal blood flow if these plaques break.
Healthcare professionals can better understand the mechanisms, develop appropriate treatment plans, and treat any concurrent cardiac conditions by recognizing the septal infarct’s relationship to other myocardial infarctions and coronary artery disease. An integrated approach that emphasizes the interconnectedness of cardiac problems is necessary for optimal management and cardiovascular health.
Special Considerations for High-Risk Groups
Septal infarct high-risk groups need specific attention. Septal infarct is more likely in older persons, especially those over 65. Age narrows and stiffens arteries, increasing the risk of blockages. Older persons may also have more comorbidities like hypertension, diabetes, and coronary artery disease, which raises their septal infarct risk.
Cardiovascular patients are another high-risk group. Diabetes, hypertension, and coronary artery disease raise the risk of septal infarction. These disorders increase coronary artery plaques, which limit blood flow to the septum.
High-risk groups must also consider lifestyle and nutritional factors that increase septal infarct risk. Smoking, inactivity, and alcohol abuse increase septal infarct risk. Saturated fats, cholesterol, and sodium can further increase the incidence of coronary artery plaques.
These high-risk categories help doctors avoid, detect, and treat septal infarction. To reduce risk and improve cardiovascular health, it emphasizes regular checkups, lifestyle changes, and tailored interventions.
Case Studies and Personal Experiences
Case studies and personal experiences can reveal how septal infarction affects people and their diagnosis, treatment, and recovery. These patient experiences help doctors comprehend septal infarct’s many symptoms and challenges.
Case studies explain patients’ medical histories, symptoms, diagnoses, treatments, and outcomes. These instances help doctors detect patterns, learn from effective interventions, and improve septal infarct management.
Septal infarct survivors can also offer insights. These anecdotes show how the illness affects individuals and their families emotionally, physically, and psychologically. They describe the diagnosis, lifestyle modifications, and recovery. Hearing patient stories helps doctors empathize and provide patient-centered treatment.
Case studies and personal experiences also advance medical research. They offer real-world examples to improve diagnosis, treatment, and patient outcomes. Sharing these experiences can help encourage others facing similar issues.
Case studies and personal experiences can help healthcare practitioners understand septal infarct, improve clinical practice, and provide better patient care. These narratives also promote septal infarct awareness and community.
Conclusion
Septal infarct, a form of myocardial infarction, damages the heart’s septum. To identify and treat septal infarct, you must understand its mechanism and clinical presentation. Recognizing risk variables such as age, gender, prior cardiovascular diseases, and lifestyle allow focused prevention and early intervention. Identifying symptoms like chest pain, shortness of breath, and others allow for immediate medical care and treatment. Electrocardiograms, echocardiography, and imaging help confirm the diagnosis. Medication, surgery, and lifestyle changes reduce septum damage, manage symptoms, and improve heart function. High-risk populations like elderly persons and those with cardiovascular diseases receive tailored care and support. Case studies and personal experiences help medical researchers understand septal infarct. Healthcare providers can enhance septal infarct identification, management, and outcomes by addressing these factors. A multidisciplinary approach to septal infarction improves heart health and quality of life.